9 Everyday Habits That Will Keep Eczema Flare-Ups at Bay
As a child, I suffered from a severe outbreak of eczema, a chronic skin condition characterized by very dry, itchy skin that also has rashes. At the time, the treatment options were limited: I ended up being covered in a tar-based ointment for a number of years. Children can be quite cruel, and the experience of being teased for such a visual manifestation of a disease outside of my control became the driving force behind why I pursued dermatology. I wanted to help people who were living with skin diseases and conditions to have a better quality of life than I did at that time.
Eczema is commonly referred to by dermatologists as “the itch that rashes,” and this is what distinguishes it from simply dry skin. People with eczema tend to be more prone to allergies as well. The itching is driven by a hypersensitivity to environmental allergens, which leads to an overactive stimulation of the nerves. The dryness is due to an imbalance of the key oils which keep the skin healthy.
Today I am a referral-only clinical dermatologist, and I see a lot of patients struggling with eczema. Often they come to my office with nowhere else to turn. Unfortunately, eczema is not curable. However, it can be controlled. My philosophy is to look at each issue holistically. I try to ask the question: What are all of the possible things in a person’s life that could be impacting how quickly they experience relief? Then I try to address all of those factors in creating a customized regimen for my patients. Each patient is different, so I recommend a wide variety of prescription and at-home therapeutic options.
Here are some of the most common (nonprescription) tips that I provide to my patients:
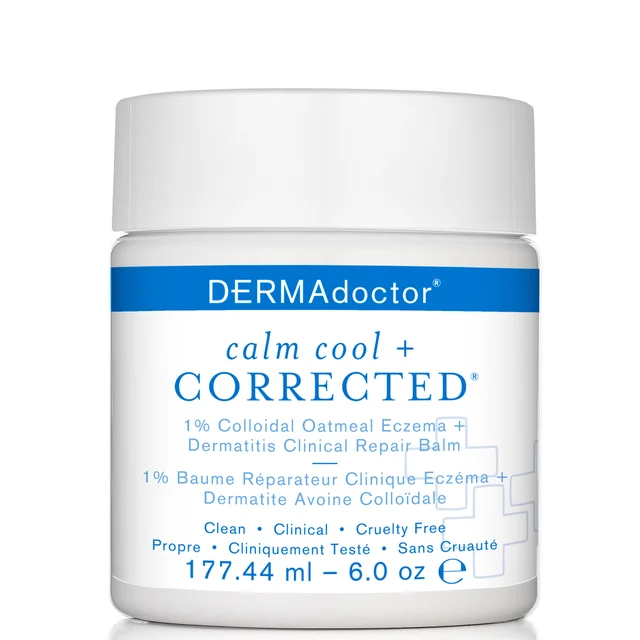
1. Use a skin care product that is
2.
3. Avoid hot temperatures, including very hot water while bathing.
4. Eat aprotein-rich diet high in anti-inflammatory and antioxidant nutrients.
5. Avoid caffeine, alcohol, chocolate and spicy foods.
6. Consider taking oral supplements that may help ease the symptoms, including vitamins C and E, flax, borage oil, iron and green tea.
7. Usefragrance-free laundry detergents and softeners. Do not use dryer sheets.
8. Clean out the air ducts in your home every six months.
9. Avoid costume jewelry—the metal nickel can be particularly irritating.
These recommendations are not meant to take the place of another physician’s specific recommendations regarding a specific treatment regimen. My goal is to help my patients feel better so they can live their lives more fully, and my hope is that some of these tips will do the same for you or someone you know.
* Content on this blog post is not considered a medical advice. Please see a physician before making any medical or lifestyle changes.*

From the latest hair and makeup trends to the best solutions for your skin issues, we've got all your beauty concerns covered!
Related Posts

6 Things Dermatologists Wish You Knew Before Buying Your Moisturizer